Study shows: Antibiotic prescribing often not in line with national guidelines
10.11.2025 - According to an analysis of over 52,000 antibiotic prescriptions within the Sentinella network, one in five prescriptions deviate from the national guidelines, especially for sinusitis and pharyngitis. In spite of the introduction of new national guidelines in 2019, only limited improvements have been seen.
The FOPH Sentinella surveillance system is a network consisting of primary care physicians (participating on a voluntary basis), continuously providing data on selected diseases and health topics for public health monitoring in Switzerland. Since 2001, the antibiotics study has been carried out within Sentinella in order to obtain a better picture of antibiotic prescribing practices in Switzerland for implementation of the Strategy on Antibiotic Resistance (StAR). A special feature of the data from the Sentinella study is that – unlike other systems for monitoring the use of antibiotics – it also includes the indications for which antibiotics have been prescribed.
A team of researchers from Lausanne and Bern has now analysed Sentinella data for the first time in such a way as to determine levels of adherence to the national guidelines published in 2019 by the Swiss Society of Infectious Diseases (SSI). Appropriate choice of antibiotic treatments is essential in order to limit the development of resistance. For this study, over 52,000 antibiotic prescriptions reported in the Sentinella network from 2017 to 2022 were analysed.
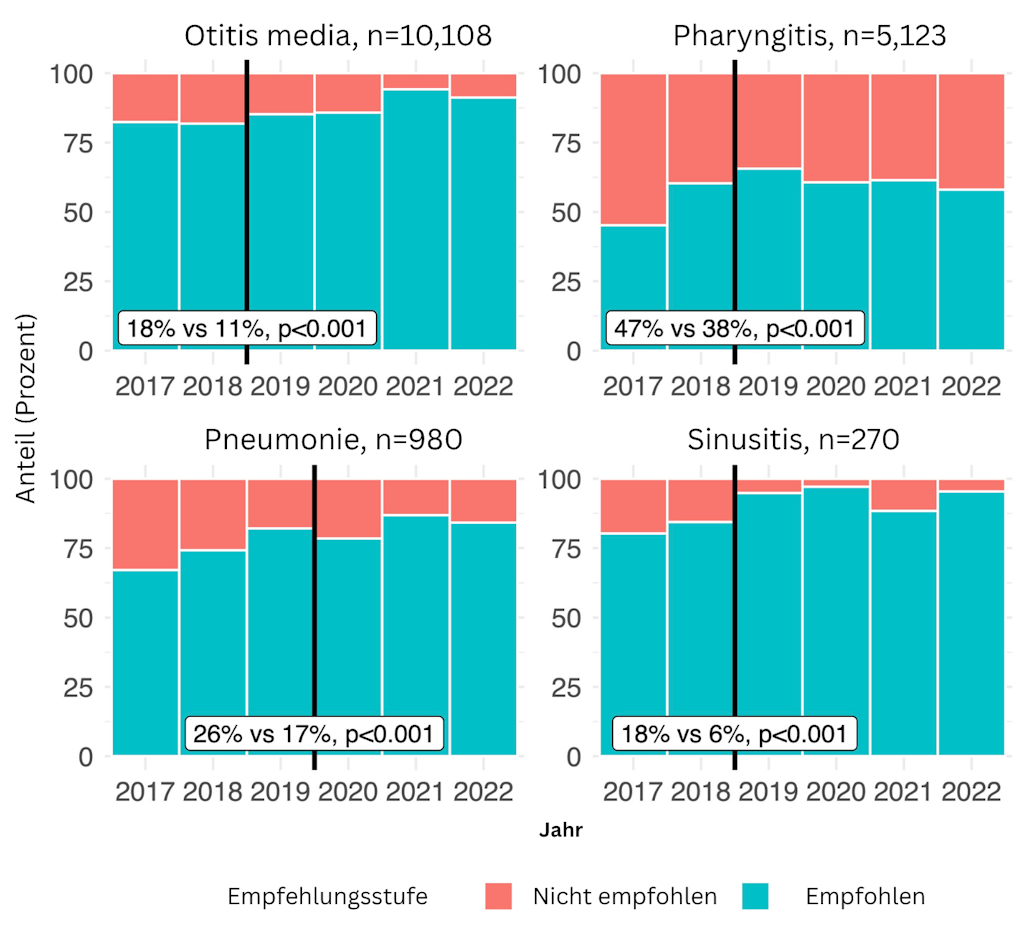
Figure 1. Proportion of recommended/non-recommended antibiotic prescriptions by clinical indication since the introduction of national guidelines.
The results show that almost one in five prescriptions are not in line with the guidelines – 18% for adults and 19% for children. This means that the antibiotic prescribed is neither the recommended first-line treatment nor one of the recommended alternatives. Certain indications show particularly high non-adherence rates, especially sinusitis in adults (39%) and pharyngitis in children (38%) (see Figure 1). The most common non-recommended antibiotic classes prescribed in adults were beta-lactamase inhibitors in combination with penicillins for pharyngitis (24%) and macrolides for sinusitis (18%).
In addition, in nearly all clinical indications among adult patients, second-line antibiotics were more frequently prescribed than the recommended first-line options. While it cannot be concluded from the Sentinella data that these prescriptions are inappropriate, the high proportion does suggest that second-line antibiotics are also prescribed for cases in which they are not recommended by the national guidelines.
Figure 2 : Change in the proportions of recommended and non‑recommended antibiotic prescriptions before and after the introduction of national guidelines in adults (a, above) and in children (b, below).
The introduction of national guidelines has led to improvements in some cases: for example, a marked decrease in the proportion of non-recommended antibiotics was seen for sinusitis (48% → 39%) and pneumonia (19% → 15%) in adults, and for all indications in children. However, the proportion of non-recommended antibiotics increased for pharyngitis in adults (22% → 29%) (see Figure 2).
A multivariate analysis revealed a number of factors associated with an increased likelihood of inappropriate antibiotic prescribing: clinical indication (particularly pharyngitis), older age of physicians, specialty (general internal medicine as opposed to paediatrics) and favourable patient’s attitude towards antibiotic prescription as perceived by the physician.
These results suggest that the mere publication of guidelines is not enough to ensure systematic implementation. In order to improve adherence, implementation strategies need to be strengthened, for example, by facilitating the integration of guidelines into electronic practice information systems, by providing specific information at continuing education events, and by involving primary care physicians in the development and updating of guidelines to ensure that they are adapted for use in the field.