When should – and shouldn’t – antibiotics be prescribed?
10.07.2024 - Time and again, doctors face the dilemma: should or shouldn’t they prescribe antibiotics for their patients? The Bern Institute of Primary Health Care (BIHAM) has been steadily developing tools since 2020 that should help GPs make such decisions in their daily professional lives. These tools have been available for five common conditions since 2023. And they’re being increasingly embraced within the medical world.

Despite the continued growth of antimicrobial resistance, antibiotics are still often unnecessarily prescribed in primary healthcare – even though the commonest infections are self-limiting, i.e. they will resolve spontaneously without treatment or intervention. Some 80% of all antibiotic’s prescriptions are for five such self-limiting or viral infections:
- acute otitis media (middle ear infection)
- urinary tract infection
- tonsillopharyngitis (sore throat)
- sinusitis/rhinosinusitis
- acute infectious cough.
Simplified decision-making
Between 2020 and 2022 a research team from the Bern Institute of Primary Health Care (BIHAM) developed a number of information and consultation tools for the use of GPs with their patients. The work was conducted as part of Switzerland’s national strategy on antibiotic resistance (StAR), and with FOPH funding. The tools were devised and developed in collaboration with a diverse interprofessional group of specialists from the epidemiology and infectiology fields. This group also included patients, experts from various specialist associations and representatives from the Swiss Patient Safety Foundation. The tools were developed in accordance with the existing guidelines of the SSI1 and on the basis of participative research and scientific findings on behavioural change. The relevant literature confirms that simple structured presentations of evidence can benefit both specialists and patients alike.2-4 These patient-appropriate tools for GPs’ use promote joint decision-making with the patient in the course of the consultation and facilitate the discussion of possible antibiotic treatments.
The BIHAM began its work with documents on simple urinary tract infections, acute otitis media and tonsillopharyngitis. With strong demand seen for these initial documents, the BIHAM team went on to develop similar documentary tools for acute sinusitis and acute infectious cough, the latter with substantial support from the Department of Infectious Diseases of the University of Lausanne. All these documents are freely available in German, French, Italian and English on the BIHAM website.
A moderation guide has also been developed with and for physicians. This guide should help quality circle participants use the new tools, and should also encourage such participants to enhance their dialogue with their patients, with the overall aim of achieving a joint decision-making process.
The tools developed
The information boards cover all key areas of the condition concerned such as its epidemiology, red flags, diagnostics and symptomatic and antibiotic treatments, which are all presented using colour-coded boxes. In addition to all the key data on the epidemiology concerned, the board’s ‹Epidemiology› section also includes the classification and the pathogenesis of the disease, along with all key supplementary information.
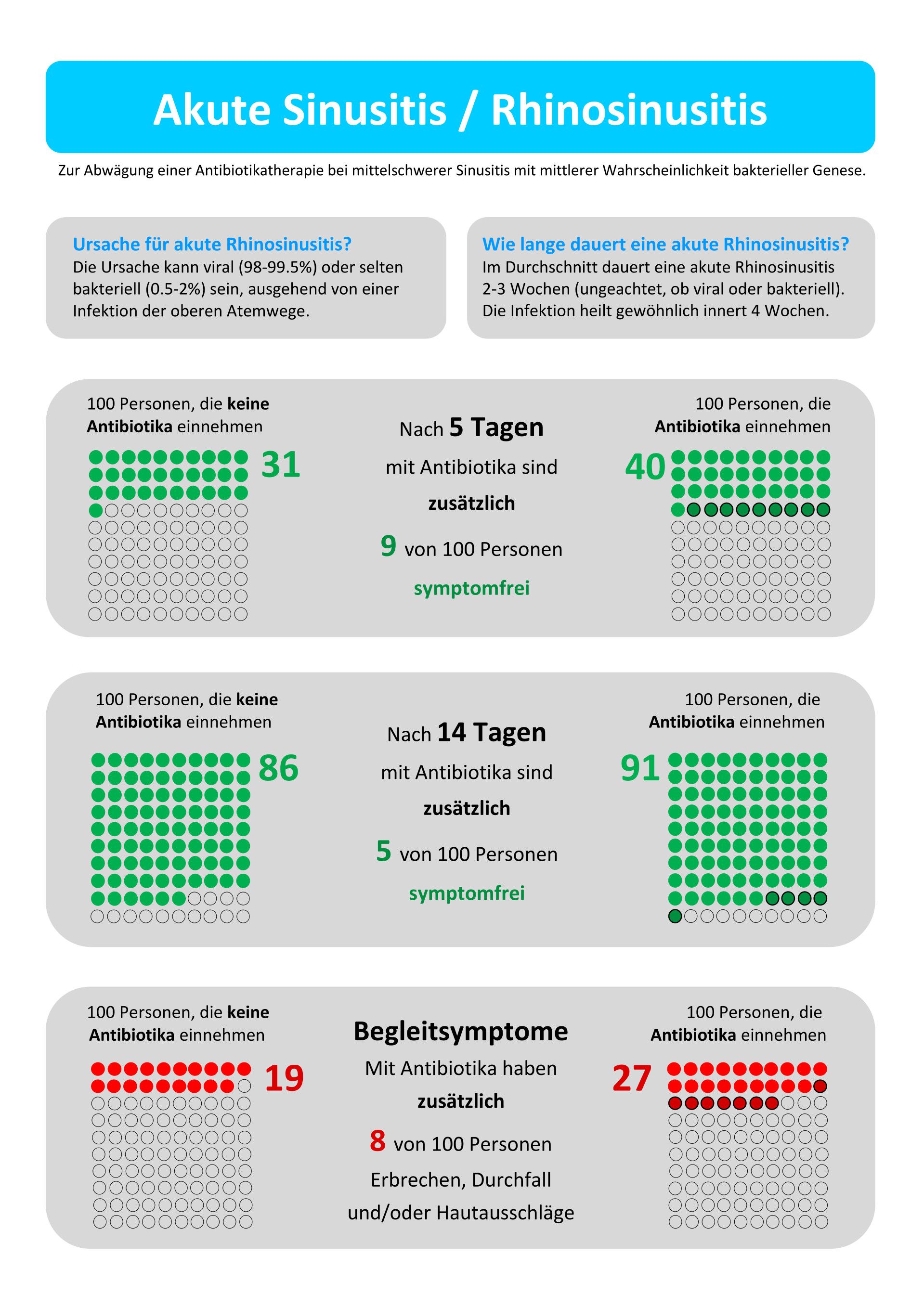
The clinical encounter support tools (CESTs) present the condition’s treatment options with or without antibiotics in graphic form, to help the physician and their patient come to a joint decision on whether an antibiotic treatment should or shouldn’t be used. Below is a sample CEST for acute sinusitis/rhinosinusitis. This and all further project documents can be viewed on and downloaded from the BIHAM website.
Healthcare provider Medbase has developed an online learning tool that should be made available to all physicians. The tool has already been trialled with success in an online workshop with interactive Mentimeter questions.
An ever-growing impact
The project has come to unexpectedly involve and impact more and more professional groups within the healthcare sector as its tools have been developed. Pharmacists, for example, have also been enlisted to distribute the documents concerned. One Master’s thesis in pharmacy at the University of Bern has already been devoted to the project; and the project’s documentation has also been further refined to meet pharmacists’ particular needs.
Interest in the project has been substantial, too, both within and beyond Switzerland. The project tools have featured in brief presentations and poster sessions at various conferences,5 where they have garnered a strongly positive response. Two graduate medical students currently working on their doctorates will also be publishing articles on the project in 2024, one in a Swiss and one in an international publication.
What next?
The distribution of the project’s documentation at Medbase’s medical centres and quality circles is currently being evaluated. Some 120 GPs working in 19 different practices have already held workshops and quality circles using these documentary tools. The next few years should also see an analysis conducted of antibiotics prescriptions based on insurance company data, which will be co-financed by the SSGIM, SWICA and the BIHAM.
References:
- Diseases, S.S.f.I. SSI Guidelines. 2022 [cited 23.03.2024.]; Available from: https://ssi.guidelines.ch/
- Coxeter, P., Del Mar, C. B., McGregor, L., Beller, E.M., Hoffmann, T. C. (2015). Interventions to facilitate shared decision making to address
antibiotic use for acute respiratory infections in primary care. The Cochrane database of systematic reviews,2015(11):Cd010907. - Bakhit, M., Del Mar, C., Gibson, E., Hoffmann, T. (2018) Shared decision making and antibiotic benefit-harm conversations: an
observational study of consultations between general practitioners and patients with acute respiratory infections. BMC family practice,
19(1), 165. - Rohrbasser, A., et al., Understanding how and why quality circles improve standards of practice, enhance professional development and Increase psychological well-being of general practitioners: a realist synthesis. BMJ Open, 2022. 12(5): p. e058453.
- These are appearances at the following conferences:
- EQUiP-Konferenz (European Society of Quality and Safety in Primary Care), Frühjahr 2023 in Dublin
- SGAIM-Konferenz, Herbst 2023 in Zürich
- Veranstaltung «Antimicrobial Stewardship in Ambulatory Care Platform (ASAP)», April 2024 in Freiburg
- SGAIM Konferenz, Frühjahr 2024 in Basel
- International Shared Decision Making Conference (ISDM), Sommer 2024 in Lausanne.

